Introduction:
Genital warts, caused by the human papillomavirus (HPV), are a common sexually transmitted infection (STI) that can affect individuals of any age or gender. These small growths on the genital and anal areas can cause discomfort and emotional distress. However, with advancements in medical science, various treatment options are available for genital wart removal. In this comprehensive guide, we will explore the causes, symptoms, and effective removal methods for genital warts.
Understanding Genital Warts:
Causes and Transmission:
Genital warts are primarily caused by specific strains Genital warts removal of HPV, with HPV types 6 and 11 being the most common culprits. The virus is transmitted through sexual contact, including vaginal, anal, or oral sex, as well as through close skin-to-skin contact. The risk of developing genital warts increases with multiple sexual partners and unprotected sex.
Symptoms:
Genital warts may appear as small, flesh-colored bumps or clusters on the genital and anal areas. They can be raised or flat, and in some cases, may cause itching, burning, or discomfort. It is essential to note that not all individuals infected with HPV will develop visible warts, making regular screenings and HPV vaccinations crucial for prevention.
Genital Wart Removal Options:
Topical Treatments:
Topical medications are often the first line of defense against genital warts. These medications, such as imiquimod and podofilox, work by stimulating the body's immune system to target and eliminate the virus. Application instructions and duration may vary, and it is crucial to follow the prescribed regimen.
Cryotherapy:
Cryotherapy involves freezing the genital warts using liquid nitrogen. The frozen warts eventually fall off, allowing new, healthy skin to replace them. This in-office procedure is effective, but multiple sessions may be required for complete removal. It can cause temporary discomfort and blistering.
Electrosurgery:
In electrosurgery, a healthcare professional uses a high-frequency electrical current to cut or burn off genital warts. This procedure is typically performed in a clinic or hospital setting, and local anesthesia may be administered to minimize discomfort. Electrosurgery is effective, but it may leave scars in some cases.
Surgical Excision:
Surgical excision involves physically cutting out the genital warts. This method is reserved for larger or more stubborn warts. Local or general anesthesia may be used, and recovery time varies depending on the extent of the procedure. Scarring is possible, but complications are rare.
Laser Therapy:
Laser therapy utilizes a focused beam of light to target and destroy genital warts. This outpatient procedure is effective for both external and internal warts. Laser therapy may require local or general anesthesia, and recovery time is generally shorter compared to some other surgical options.
Preventive Measures:
Vaccination:
The HPV vaccine is a highly effective preventive measure, protecting against the most common HPV types, including those responsible for genital warts. Vaccination is recommended for adolescents and young adults, but it can also be administered to individuals up to age 45.
Safe Sexual Practices:
Consistent and correct condom use can reduce the risk of HPV transmission. Limiting sexual partners and practicing safe sex are essential preventive measures. Regular screenings and communication with sexual partners about STI status also contribute to prevention.
Conclusion:
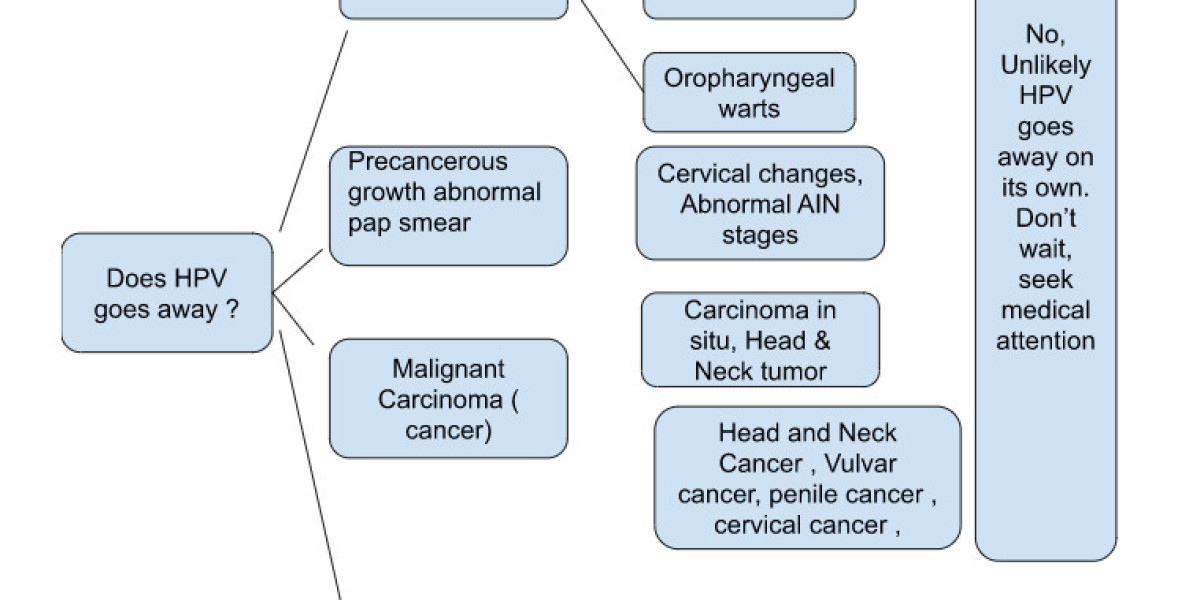
Genital warts can be a challenging and emotionally distressing condition, but with advancements in medical treatments and preventive measures, individuals can effectively manage and remove these growths. Seeking professional medical advice is crucial for proper diagnosis and personalized treatment plans. Additionally, adopting safe sexual practices and staying informed about HPV vaccinations can contribute to the overall prevention of genital warts and other HPV-related complications.