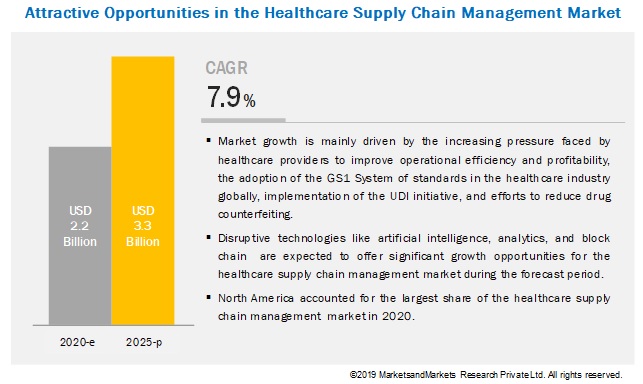
The healthcare industry is witnessing a significant transformation, with the global healthcare fraud analytics market on the rise. According to a recent report by MarketsandMarkets, the market's revenue was estimated at $1.5 billion in 2021, and it is projected to reach an impressive $5.0 billion by 2026. This growth is set at a remarkable compound annual growth rate (CAGR) of 26.7% from 2021 to 2026.
Download PDF Brochure-https://www.marketsandmarkets.com/pdfdownloadNew.asp?id=221837663
The healthcare fraud analytics market is driven by several key factors that are shaping its landscape. Let's delve into some of the major dynamics influencing this market.
Driver: Increased Number of Patients Seeking Health Insurance
One of the driving forces behind the growth of the healthcare fraud analytics market is the surge in the number of individuals seeking health insurance. This trend is observed globally, with the aging population, increased healthcare expenditure, and rising disease burden contributing to the expansion of the health insurance sector. In the United States, for example, there has been a significant reduction in the number of citizens without health insurance, from 48 million in 2010 to 28.6 million in 2016. This trend is attributed to various factors, including favorable government initiatives and increased affordability of health insurance for the middle class.
Emerging markets, particularly in Asia, are also promising areas for growth in health insurance coverage. Government initiatives, rising investments, and higher income levels are driving the adoption of health insurance in these regions. Regulatory changes, such as mandatory medical insurance in the UAE, are further fueling the growth of the health insurance market.
Restraint: Limitations in Data Capturing Process in Medicaid Services
While the healthcare fraud analytics market is experiencing rapid growth, it faces challenges related to data accuracy and completeness, particularly in the public sector. In the United States, national Medicaid data has been found to have shortcomings that could hinder the detection of fraudulent claims. Inaccurate and incomplete Medicaid data can lead to wasted resources and billions of dollars lost due to fraudulent activities. Overcoming these limitations is essential for the effective detection and prevention of healthcare fraud.
Opportunity: Emergence of Social Media in Healthcare
The healthcare industry is undergoing a transformation driven by the increasing popularity of healthcare communication through social media. Social media platforms have become hubs for seeking health information, and they facilitate two-way communication between patients, healthcare providers, and other stakeholders. This vast network of healthcare influencers, organizations, and individuals generates a wealth of healthcare data that, if analyzed effectively, can improve treatment efficiencies and health outcomes.
As a result, there is a growing demand for data aggregation and analytical tools in the healthcare fraud analytics industry. Social media data can be a valuable resource for detecting healthcare fraud, and leveraging this data presents significant opportunities for the industry's growth.
Challenge: Time-Consuming Deployment and Frequent Upgrades
Deploying fraud analytics solutions can be a time-consuming process, involving the creation of user interfaces, databases, predictive models, and continuous monitoring. Data analysts often need to run algorithms repeatedly to identify the most effective predictive model, which can lead to time wastage. Additionally, fraud analytics software requires frequent updates to keep up with evolving tactics used by fraudsters. These factors contribute to the overall cost of fraud analytics solutions.
The healthcare fraud analytics market is categorized based on solution type, delivery model, application, and end-user. Descriptive analytics is the dominant solution type, while insurance claims review is the leading application segment.
Geographically, North America is expected to dominate the healthcare fraud analytics market from 2021 to 2026. Factors such as a high number of people with health insurance, increasing healthcare fraud, favorable government initiatives, and technological advancements contribute to the region's leadership in this market.
Key players in the healthcare fraud analytics market include IBM Corporation, Optum, Inc., Cotiviti, Inc., Change Healthcare, Fair Isaac Corporation, SAS Institute Inc., and many others.
Download PDF Brochure-https://www.marketsandmarkets.com/pdfdownloadNew.asp?id=221837663
In conclusion, the global healthcare fraud analytics market is experiencing significant growth, driven by factors like the increasing demand for health insurance, the emergence of social media in healthcare, and the need for more robust fraud detection and prevention measures. However, challenges related to data accuracy and deployment efficiency must be addressed to fully harness the potential of this growing market.